Blog 4: The hospice movement
As I mentioned in a previous blog I had attended two hospices for teaching as a medical student. How strange it felt to walk through the doors of St Margaret of Scotland hospice to interview for a specialty doctor job.
I had done a bit of research into the hospice movement and how hospices had originally come into existence. The history is quite complex and relates back to the "foundations of palliative care" blog.
Many associate the origin of hospices with Dame Cicely Saunders and the establishment of St Christopher's house in London circa 1967. Indeed Dame Saunders was the original pioneer of the modern palliative care ethos, however there were hospice based establishments prior to this.
St Christopher's Hospice 1970's

Madame Jeanne Garnier founded the Dames de Calaire in Lyon, France around 1843. This led to further centres being established in Paris and New York towards the 1900's. These settings provided care for the dying in a time when medical practice was advancing quickly towards seeking "cure". Madame Garnier had experienced the death of her husband and child, she recognised the need for places to support people to die well.
The Irish sisters of charity took note of this approach. They opened Our Lady's hospice in Dublin and St Joseph's hospice in London. St Margaret of Scotland hospice (the setting for my interview) was opened in 1950 by the Sisters of charity in Clydebank, Glasgow. Again born out of a recognition that there was a deficit in the care available for people who were dying.
The care in these early hospices focused on nursing and spiritual care. It wasn't until 1967 and Dame Saunders vision that a role for doctors was envisaged. Recruiting medical practitioners into the hospice brought about the beginning of what we now recognise as palliative symptom control. The early work done was pioneering, there were no guidelines and no peer reviewed evidence. A new specialty was being created and Dame Saunders was performing prospective research along the way. Her books and teachings are still as fresh to read today as the back then. She enrolled the help of Robert Twycross to further study pain and symptom control. Twycross remains one of the leading experts in palliative care prescribing and his books are used daily by palliative care clinicians as guides. I have a copy of the current palliative care formulary (PCF7) on the table in front of me right now.
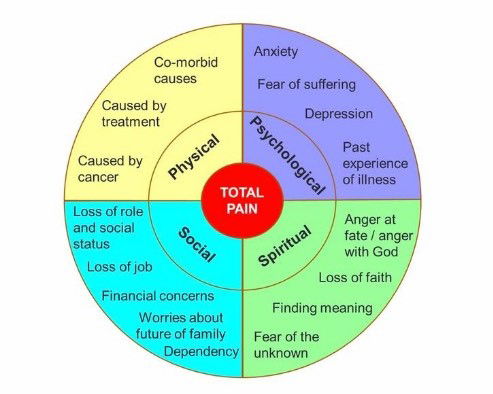
Dame Saunders introduced the concept of total pain. An idea that deserves a blog on it's own. In simple terms pain is not just physical. It consists of many dimensions which interact and fuel one another. It taught me why pain killers don't always work. There are no receptors in the brain for spiritual or financial distress. The diagram below gives an outline how complex pain can be. The approach to alleviating distress needs to go beyond the physical domain.
Total pain dimensions
This concept led to the recognition that a multi-disciplinary team approach was needed to fully address suffering and pain. A revolution in symptom control followed with greater understanding of the potential benefits and limitations of medication use towards end of life. Holistic assessment of patients on admission was now performed with a paradigm shift in the understanding of what can cause distress beyond the illness itself. The role of adjustment reactions to bad news, anxiety, depression and hopelessness in symptom burden was realised. Spiritual pain in the form of guilt, anger, fear of the dying process and what comes after death was explored. The role of an individual's social, cultural, religious and even financial dimensions all come into the holistic assessment. The first bereavement assessment and support network evolved from this work. In 1969 the in-patient unit at St Christopher's evolved to provide end of life care support in people's own houses- the first community palliative care team.
Dame Saunders and her team helped spread the word far and wide: Publishing books, lecturing abroad and advocating for these approaches within the medical profession.
Dame Saunders died in St Christopher's on 14th July 2005. Although I never met her I like to think of her as having a tender, caring bed side-manner while being fiercely intelligent and a powerful advocate for her patients, staff and specialty.
(Dame Cicely Saunders laughing with a patient)

I got the job. I remember being phoned by Professor John Welsh with the good news. I worked my notice as an acute medical trainee at Crosshouse hospital and started work as a palliative care doctor in 2016.
St Margaret of Scotland hospice is based in Clydebank in Glasgow. The hospice covers a wide range of socioeconomic areas. Clydebank itself was a shipbuilding town. It suffered horrendous bombing in WWII. The "Clydebank Blitz" in 1941 killed 528 people and left thousands homeless. There are still bomb craters on the banks of the river Clyde ( I have personally fallen into one of these looking for a lost golf ball). Other Clydeside working class areas include Drumchapel and Yoker. Moving inland the hospice covered the more affluent areas of Bearsden and Milngavie (pronounced mill-guy).
Clydebank blitz 1941

I soon learned about the impact of socioeconomic status on health equality. The patients from the old shipbuilding areas had higher rates of mesothelioma (caused by asbestos in the shipyards), lung cancer, throat cancer( linked with smoking and alcohol use), COPD (smoking related lung disease),cardiovascular disease and tended to die younger. Patients from more affluent areas may be more likely to live longer and have conditions such as prostate cancer and dementia. There are well established links between deprivation and ill health although many cancers do not discriminate between social or financial status. I'll cover my work in the community more in a future blog.
As I mentioned in blog 3 "Foundations of palliative care" I had never really seen patients in a hospice setting. I had looked after many seriously unwell people in hospital and been involved in the care of numerous people who had died.
So here I was. Fairly naïve to the workings of a hospice but with a good grounding in general medicine. I'm glad I did those years of medical training, I was going to need them more than I had realised.
As a hospice doctor I found myself much more responsible for complete patient care. Yes I managed symptoms and performed holistic assessment but I also dealt with a huge range of other medical situations. People admitted to a hospice will come with a medical history. They may be diabetic, have Parkinson's disease, multiple sclerosis, asthma, bipolar affective disorder, irregular heart rhythms , tracheostomies, skin conditions, eye conditions....really any medical, surgical or psychiatric condition you can think of. It is vital that these conditions are managed properly as if they are treated sub-optimally the person may suffer additional distress or die from one of these previously stable ailments.
I gained a new knowledge of how to reduce and stop medications. There is a medical concept known as "polypharmacy". This term simply means that someone is taking lots of different medications. There is convincing evidence that polypharmacy leads to reduced quality of life, increased episodes of confusion and dangerous falls particularly in the elderly and those who are more frail. Factor this in with people who are becoming less well towards the end of their life and you have the potential for serious problems. It is normal for people who are in the last days-weeks of their life to eat less. Imagine having a cupful of potentially unnecessary tablets placed in front of you four times a day when this is occurring. This can put a lot of pressure on patients, and over medicalise their last days, not to mention the unpleasant process of trying to swallow them.

Many medications can be stopped safely. A lot of the medications used in modern medicine are used to prevent disease. These work over many months or even years. A classic example is the group of cholesterol lowering drugs known as Statins. Stopping any statin in the last weeks of life will cause no harm, in fact there is some evidence that it may improve quality of life for some patients. Palliative care clinicians do not stop medications without careful consideration. There is guidance available on how to do this safely. Some medications need to be slowly reduced to avoid withdrawal effects. Drugs such as anti-depressants, opioids and steroids cannot be stopped too quickly as this may result in distressing physical and psychological symptoms.
There are specific guidelines for managing some general medical conditions in those approaching end of life. A great example is the work done by Diabetes UK that provides superb step by step guidance on how to safely manage patients who may be on insulin or other diabetic medications. I've provided the link below as it is one of my favourite guidelines. It is so user friendly, I wish all guidelines were as approachable.
EoL_Guidance_2018_Final.pdf (diabetes.org.uk)
I have a fascination with how drugs work. I'm a bit of a pharmacology geek on the side. I found myself learning at an exponential rate. Every medication I prescribed for symptom control I wanted to know more about. How was it discovered, how did it work, how long did it work for, what were the side-effects and how did it interact with all these other medications people were on already.
I had the pleasure of working with two great palliative care pharmacists Elayne and Carolyn during my time in Glasgow. Pharmacists are vital in palliative care, for so many reasons I couldn't list them all but here are a few: simplifying complex drug regimens, highlighting dangerous drug interactions, sourcing rare medications at short notice, providing up to date prescribing guidelines, checking doctors' prescribing (and oh boy do we need this support) and helping patients/families understand their medications at the point of discharge. I must have driven them mad with all my questions but they always got back to me with a solution.
Many of the drugs used in palliative care are what are called "off-license" prescriptions. This means they are being used in a way that they were not originally designed for (licensed for) . This can be when a drug is used for a different condition, when it is used at a different dose, given via a different route or for a different duration of time. Although common practice across many areas of medicine this approach needs extra care. Our palliative care pharmacists play a pivotal role in this area.
One of the reasons we use so many off-license medications in palliative care is the lack of research resources directed towards the specialty (as far as I can see). As a result palliative care has adapted medications used by other specialties into its everyday practice. Through this practice a huge range of medications have been discovered to help with distressing symptoms patients may experience.
There remains a need for more research into existing and potentially new medications used in palliative care. There are promising signs. Even something as simple as good old fashioned paracetamol still raises debate among clinicians. It appears there may be a randomised control trial (the best quality of evidence to support any research findings) on the horizon to sort out this debate.
I started my work on the in-patient wards. Working alongside Professor John Welsh I learned a whole new approach to patient care. I've covered some of the purely medical side of things in this blog but I aim to cover the holistic aspects of care in the next few blogs. The next blog will cover the importance of communication in palliative care.
St Margaret of Scotland Hospice, Clydebank.
